Why do varicose veins happen?
Risk factors for varicose veins
What can happen with varicose veins?
Varicose vein treatments
Varicose veins are superficial veins that have become abnormally distended and tortuous. They can range in size from 3mm to 2-3cm!
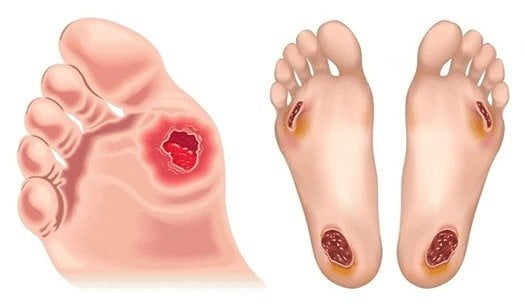
Venous disease can vary in severity. Mild cases may present as spider veins. Advanced cases can cause swelling, discolouration, and even breakage of the skin, known as venous ulceration.
Our superficial and deep venous systems bring deoxygenated blood back to the heart. This blood has been used by our muscles, skin, etc.
Varicose veins occur when the valves inside the vein become ‘incompetent’ ie they stop working properly. These leaky vein valves cause back pressure in the veins below them. This pressure is most pronounced at the ankle due to gravity when we are standing.
Varicose veins, venous oedema, venous eczema (itchy, dry skin), pigmentation, and brawny scarring called lipo-dermatosclerosis can all eventually appear due to this increased pressure. Additionally, venous ulceration, which is breaks in the skin, is a potential result.
The main concern with varicose veins is aesthetic, but if left untreated, they can lead to more serious health problems such as skin breakdown, stasis dermatitis, and deep vein thrombosis.
Treatment options for varicose veins range from lifestyle modifications to minimally invasive procedures such as sclerotherapy and endovenous laser therapy. Each person’s treatment plan is tailored to their individual needs and goals. It is important to talk to your doctor about any varicose veins you may have, as early diagnosis and treatment can help reduce your risk of long-term complications.

Risk factors for varicose veins:
Varicose veins are more common in women. They can be inherited. If your parents had varicose veins, you can thank them. Other common risk factors include pregnancy, obesity, menopause, ageing, leg injury, history of DVT.
In Southeast Queensland, the humidity and warmth make existing varicose veins swell even more. This can be very uncomfortable for many patients who need to wear compression garments. Varicose veins can be cosmetically upsetting for some patients, in others they cause aching & fatigue in the leg. With more advanced venous disease you can see freckling/pigmentation, venous eczema (skin irritation) & scarring (lipodermatosclerosis).
With more severe disease, varicose veins also be associated with:
- Cellulitis (bacterial infection of skin)
- Superficial thrombophlebitis (blood clots near the skin, in superficial veins only)
- Mild increased risk in DVT (deep venous thrombosis/clot)
- Non healing wounds or venous ulcers
What are my options with varicose vein treatments?
Conservative:
- Lose excess weight
- Elevate legs when sitting
- Wearing fitted compression garment (Grade 2 or higher)
- Exercising
- Avoid very hot showers; can worsen spider veins
In order to adequately assess what surgical options are appropriate and to define your individual venous disease, a good quality venous incompetence ultrasound study will be necessary. This can be ordered by your GP prior to seeing Dr O’Donnell as this will save you time. This usually takes 30-45 mins to complete on each leg.
Non surgical procedure:
Sclerotherapy: this involves injection of different types of solutions into spider veins or small varicose veins to stop the filling. It works in 80% of patients but often needs to be repeated & can take several sessions.
Surgical procedures:
- Phlebectomy: removing superficial bulging veins through multiple tiny skin incisions
- Venaseal: Closing off vein with medical ‘glue’ delivered via specific catheter/device
- Radiofrequency ablation/ClosureFast: minimally invasive, no groin incision. This method uses heat therapy to close off the incompetent main veins. No synthetic material is left behind; the vein seals itself. This endovenous technique is guided with ultrasound. You can watch the video below to understand this technique better.
- Open surgical varicose veins repair- reserved for patients not anatomically suitable for minimally invasive techniques ie venous aneurysms etc
- Pelvic congestion is less common. Varicose veins in the pelvis can contribute to swelling or recurrent veins in the lower limbs.Dr O’Donnell may feel they should be assessed with ultrasounds or CT imaging. She will explain this & tailor treatment for you if necessary. To read more about pelvic congestion, please take a look at our specific section here.
Australian & New Zealand Society of Vascular Surgery (ANZSVS) advice on varicose veins
Endovenous thermal treatments for varicose veins
Chronic venous disease & venous ulcers